ULTRASOUND GUIDED CORE NEEDLE BIOPSY
ULTRASOUND GUIDED CORE NEEDLE BIOPSY
SCREENING TO DIAGNOSIS
Mammography screening is one of the major advances in breast cancer care. Early detection is the main reason that the death rate from breast cancer has declined in the United States by over 40% since 1990. However, mammography screening is far from perfect. It does not detect all cancers and does not detect all cancers at a time when cure is possible. Furthermore, screening detects benign structures in the breast that are not cancer but cannot be differentiated from breast cancer based on the imaging. In the U.S. approximately 10% of women who participate in screening are recalled for additional evaluation with additional mammographic views or ultrasound. Many of these women can be told that the additional imaging shows that there is nothing of concern and they can return to annual screening. Others may be advised that there is no immediate concern, but that they should return in 6 months to be certain that what is seen on their mammogram is stable and likely is benign, while a small percentage of women (2% of the women screened) are advised to have an imaging guided needle biopsy to determine the histology of the lesion that was found on screening. I prefer core needle biopsy rather than fine needle aspiration (FNA) cytology because the histology provided by the cores provides a more complete diagnosis than cytological analysis.
ULTRASOUND IS THE BEST WAY TO TELL A CYST FROM A SOLID MASS
When there is an indeterminate lesion that is found by screening and confirmed by additional mammographic views (if needed), the next test is almost always ultrasound. Unless, using mammography, a circumscribed structure is found to contain calcifications that layer dependently and move with gravity indicating “milk of calcium”, mammography is unable to differentiate a simple, benign cyst from a solid mass.
Ultrasound can almost always confirm when a structure, that is indeterminate on mammography, is a cyst. Simple cysts are benign and need no further intervention unless they are causing pain. In that case, an image guided cyst aspiration may be useful, but this is very unusual. Image guided cyst aspiration can be performed using the same technique as for a biopsy, but, instead of inserting a biopsy device through an introducer under ultrasound guidance, an aspiration needle is used. The needle should be attached by connecting tubing to a syringe, and while the radiologist is inserting the needle under ultrasound observation, when the lesion is penetrated by the needle, an assistant can provide suction using the syringe.

ULTRASOUND GUIDED NEEDLE POSITIONING
Whether for guiding the aspiration of a cyst, or the biopsy of a solid mass, ultrasound is one of safest, easiest, and most accurate ways to guide the positioning of a needle into a lesion. The patient is positioned supine with the ipsilateral arm positioned behind her head to flatten the breast on the chest wall. The patient can be rolled to better position the breast. The goal is to position the patient, breast, and lesion to provide the safest access for the biopsy needle. Safety is of fundamental importance. Needles should always be positioned as parallel to the chest wall as possible so that when the sample is taken, the needle tip can pass beyond the lesion without reaching the chest wall.
The patient is scanned to determine the location of the lesion and the skin is marked directly over the lesion. Then, placing the ultrasound transducer over the lesion the location is marked for the skin entry point. The skin entry point is chosen so that when the needle enters the skin the needle tip can be seen at all times under the transducer as the needle is advanced toward the lesion.
The transducer is covered with a sterile sleeve that contains coupling gel. The needle entry location is then cleaned with betadine and alcohol and a sterile drape with an opening is placed with the skin entry point in the opening.
The skin entry point is infiltrated with local anesthesia.
I prefer using an introducing needle because this facilitates multiple insertions of the biopsy needle without having to make multiple damaging passes through the breast tissues to return to the lesion for sampling. The introducer is positioned under ultrasound guidance. The ultrasound transducer is positioned so that the lesion and the needle tip can be seen at the same time. The angle that the needle is introduced is chosen so that when a biopsy needle is passed through the introducer and “fired”, the biopsy needle tip will end in breast tissue with no risk of hitting the chest wall.
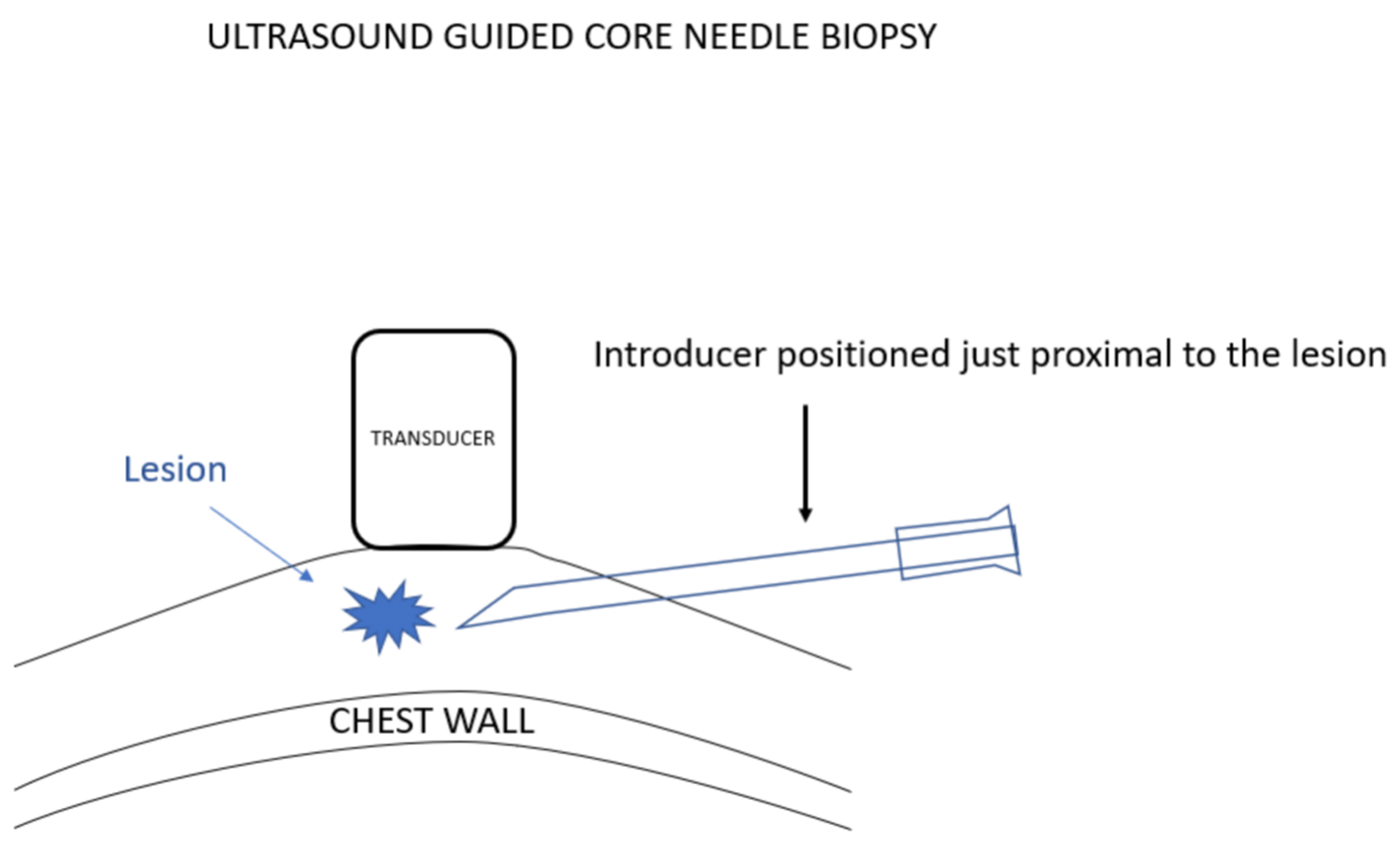
I prefer to use a spring-loaded biopsy needle because it is often difficult to push a needle into a breast lesion since the lesion often gets pushed out of the way. Tissue inertia with the spring driven rapid movement of the biopsy devise reduces the chance of this happening. Using these devices makes it important to be certain that if the tip of the biopsy device moves further than expected it will remain in the breast and will not reach the chest wall or beyond.


Multiple samples are obtained as needed. If a single sample system is used, I have a test tube with sterile saline that allows me to insert the needle and notch of the device and to wash the notch of the biopsy needle and remove the tissue sample into the saline. Thus, the biopsy needle is kept sterile and is never in contact with any preservative and can be safely passed back into the breast for the next sample. At the end of the procedure the samples that are held in the saline tube can be poured into a larger amount of preservative to be sent for pathological analysis.

When the procedure is complete, the introducing needle is withdrawn, and pressure placed over the biopsy and skin entry to provide hemostasis. Then a dressing can be applied to the skin entry site.
As with all biopsies, the pathology results should be evaluated to be certain that they are concordant with the imaging expectations and that the sampling was complete. If the results are not concordant, then an excisional biopsy should be considered.